Advanced Primary Care Management FAQ
Advanced Primary Care Management (APCM) is a new way for primary care providers to get fair compensation from Medicare for all the between-visit work they do to help and support their patients.
Here are common questions from healthcare organizations considering APCM. You can use these questions to understand what APCM is, learn more about reimbursement and billing, and evaluate if APCM is the right fit for your organization.
Advanced Primary Care Management (APCM) is a fee-for-service (FFS) Medicare program that reimburses medical practices for between-visit care. APCM is available to all Medicare patients, expanding Connected Care access to millions more people than previously qualified under other FFS programs.
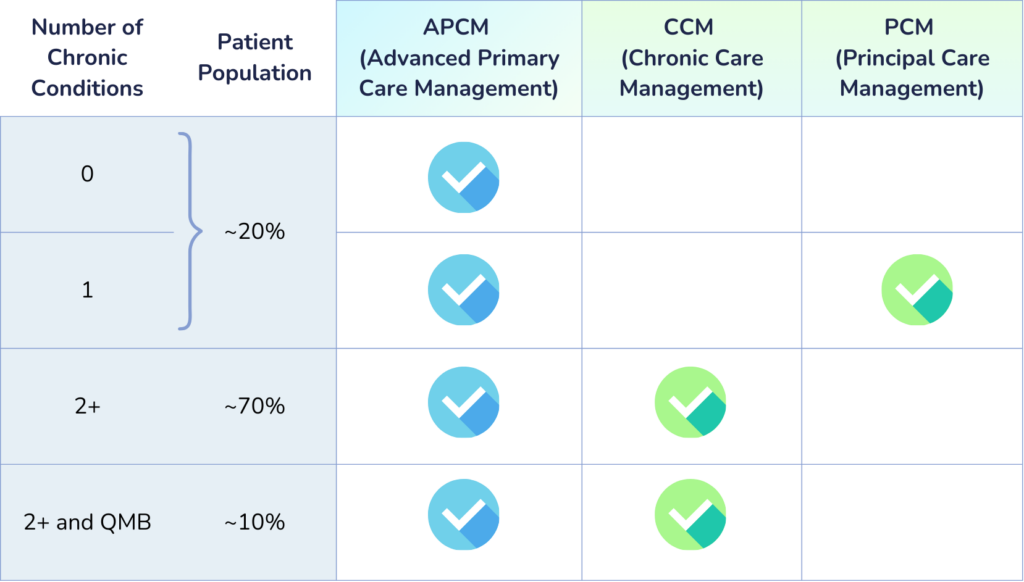
While both APCM and Chronic Care Management (CCM) are FFS Medicare programs that support value-based care (VBC) initiatives, they do have a number of significant differences. For example, CCM is only available to patients with 2+ chronic conditions, whereas APCM is available to all patients in need of proactive care. CCM also has a time requirement that APCM does not. However, there are additional requirements for medical practices to qualify for APCM reimbursement that CCM providers do not have to meet. Both APCM and CCM can be billed for the same patient concurrently, but not by the same practice in the same month. Learn more about APCM vs. CCM.
Any Medicare patient can qualify for APCM. Unlike CCM and other programs, APCM does not require a specific number of chronic conditions. Instead, APCM is available for any patient seen by the provider in the past 3 years who needs additional care between office visits. This means patients who do not have an official chronic condition diagnosis, but who are at elevated risk, can receive additional care from their providers to help maintain their health.
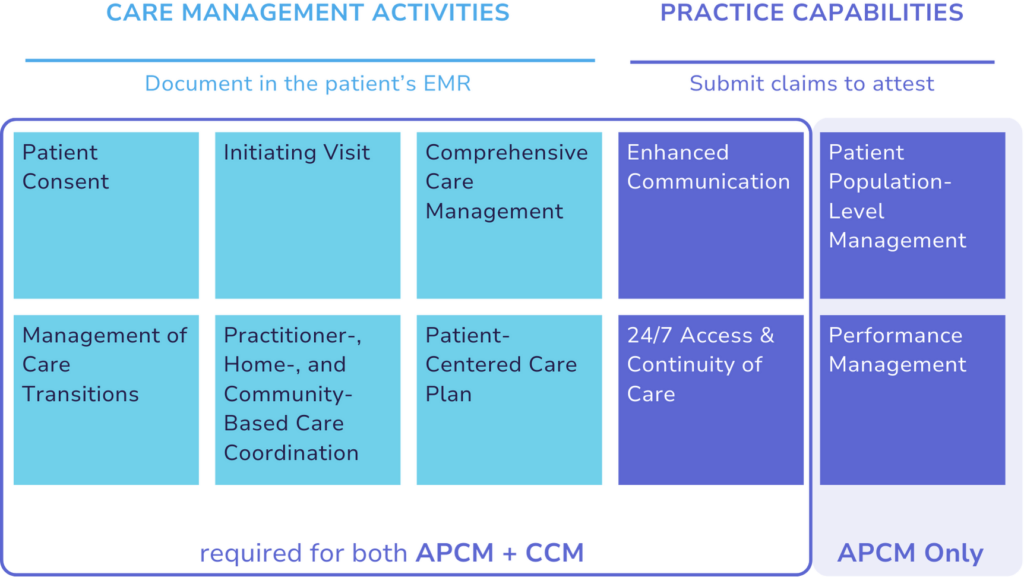
There are 10 requirements for APCM. These are split into 4 practice capabilities, and 6 care management activities. Providers must document compliance with each of these requirements to be eligible for APCM reimbursement. Some of the requirements include gaining patient consent, creating a patient-centered care plan, and providing 24/7 access and continuity of care.
Advanced Primary Care Management supports patients by delivering high quality, proactive care to help them maintain their health and manage any conditions they may have. Using APCM, providers can build trusted relationships with their patients and open lines of communication that can help care managers identify if a patient requires additional medical support. APCM is just one program designed to strengthen primary care services, which CMS believes are “fundamental to improving health outcomes, lowering mortality, and reducing health disparities.”— “Calendar Year (CY) 2025 Medicare Physician Fee Schedule Final Rule,” CMS.
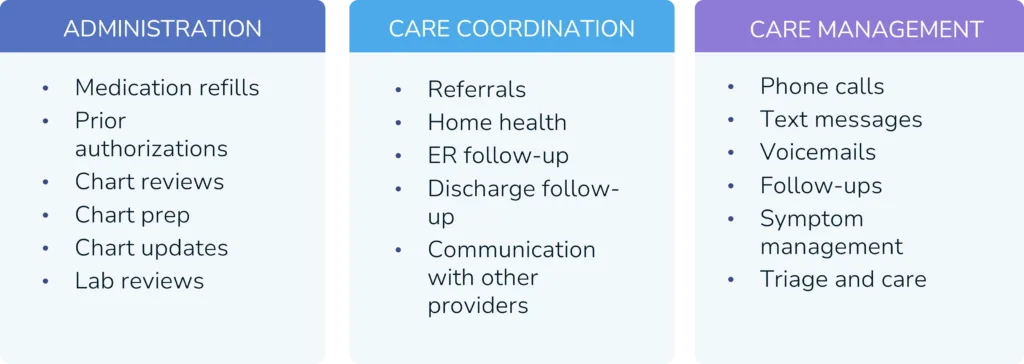
Healthcare practices are faced with an increasing workload of between-visit care activities. From triaging phone calls to refilling medications, clinical staff are busier than ever, and historically very little of that work was directly reimbursable. APCM not only makes it possible for practices to be fairly compensated for between-visit care, but also provides a framework to structure care in a more consistent way that can actually reduce administrative burden. Phamily estimates that a fully ramped APCM program should deliver $862,000 annually per 1,500 patients enrolled, at a 50% profit margin.
APCM Reimbursement & Billing
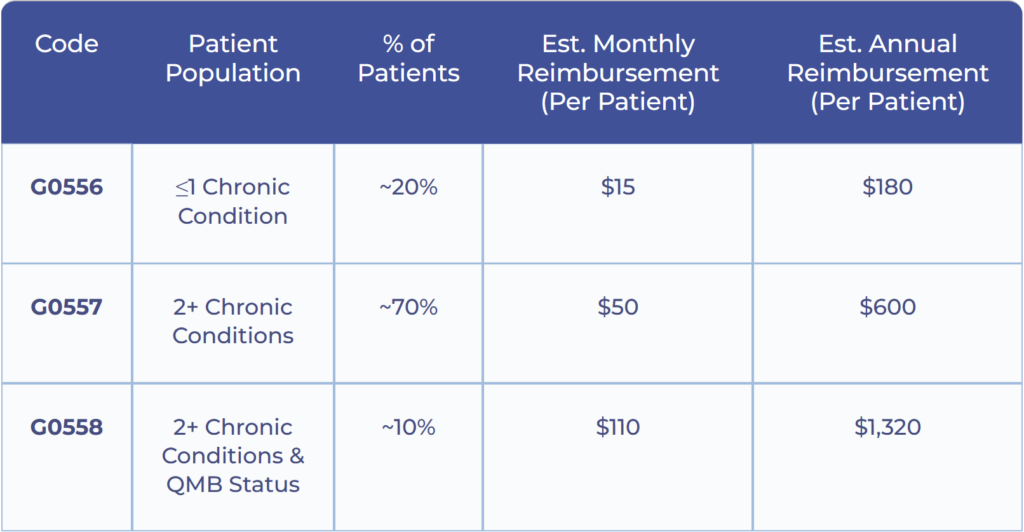
Reimbursement for APCM depends on the number of chronic conditions a patient has, and their Qualified Medical Beneficiary (QMB) status. Reimbursement starts at $15/month for patients with ≤1 chronic conditions, and is as high as $110/month for patients with 2+ chronic conditions and QMB status.
APCM is billed under three different codes, depending on the number of chronic conditions a patient has and their Qualified Medical Beneficiary (QMB) status.
Medicare Advantage plans are required to cover “all medically necessary services” covered by Traditional Medicare. The majority of MA plans cover other care management services, such as CCM, and we expect that over time, most MA plans will extend coverage to APCM. Currently, however, the only way to determine if a particular MA plan covers APCM is to submit a claim to see the response and reimbursement rate.
Reimbursement rates can vary significantly between plans. For CCM, Traditional Medicare reimburses practices at $62.58 for 20 minutes of care (99490). But we frequently see reimbursement as low as $0 or $2 and as high as $80 or even more from Medicare Advantage plans for that same 20 minutes.
Currently, Medicaid does not provide coverage for APCM. However, Medicaid does participate in other fee-for-service continuous care programs on a state-by-state basis.
While it is possible for a patient to receive both CCM and APCM in the same month, they cannot be billed by the same provider. Generally, APCM is most appropriate for primary care practitioners, while CCM is a better fit for specialty providers.
Yes, a patient can receive APCM and CCM in the same month if they are delivered by different providers. For example, a patient with chronic kidney disease (CKD) could receive CCM from their nephrologist and APCM from their primary care physician in the same month.
As with all Medicare services, patients may have an applicable copay for APCM services, depending on their plan. Many patients carry supplemental insurance, which may alleviate any out-of-pocket costs, but it’s important to help patients understand the importance of receiving between-visit care to help them maintain their health. An exception is patients with Qualified Medicare Beneficiary (QMB) status. These patients do not have a cost-sharing requirement to receive APCM.
Unlike CCM, PCM, and RPM, there is no time-based component of APCM required for billing. Instead, the 10 APCM requirements are structured to help providers deliver the best possible patient care without being obliged to track their time.
Implementing APCM
APCM reimburses practices for delivering between-visit care and support to their patients. Many practices are already doing these activities, and because of this, we have seen healthcare organizations ramp up APCM programs within 30 days. While APCM provides a framework for reimbursable activities, it crucially prioritizes care management that engages and activates patients in ways that are key to better health outcomes. Practices should think about the tools and staff they would need to meet each APCM requirement, and how to best provide high quality, consistent care between office visits. Download our APCM checklist to learn more.
Patients must consent to receiving APCM before practices can bill for the service. To properly consent a patient, practices must inform the patient:
- about the availability of services
- that only one practitioner can furnish these services
- that the patient has the right to stop services at any time
- and that the patient has potential cost-sharing requirements.
Consent only needs to be obtained once, unless the billing provider changes. It can be obtained remotely or in person, and does not need to be written. Consent must be documented in the patient’s medical record.
Yes, provided the auxiliary personnel are working under the general supervision of a billing provider and meet all other qualifying criteria. Learn more about qualifying APCM providers.
APCM extends care events beyond in-person office visits to cover a wide range of administrative duties and care management and coordination activities.
want to learn more?
get a demo
Are you a patient? Click here to learn about Phamily for patients.
Consistent care, fewer calls
Replace hundreds of monthly phone calls with weekly personalized text check-ins that patients love.
Work smarter, not harder
Headache-free auto-documenting care management, smart care plan templates and follow-up protocols.
Get a free financial model
Understand the impact of APCM on your practice with a customized financial pro forma.