Neurologists provide extensive between-visit care to their patients with chronic conditions – but only 0.37% are earning fair compensation for that care through Medicare’s Chronic Care Management (CCM) Program. This underutilized program can benefit neurology patients with two or more chronic conditions while creating a durable revenue stream for neurology practices.
KEY TAKEAWAYS:
Neurology practices have several new options to care for patients with chronic conditions or complex needs – but shouldn’t overlook the existing CCM program.
The Centers for Medicare & Medicaid Services (CMS) projects that the finalized 2024 Medicare Physician Fee Schedule will increase payments to neurology by about one percent. The American Academy of Neurology sees several positive developments in the new fee schedule to help appropriately compensate neurologists for the care of patients with complex needs.
Neurology practices can also assist patients with principal illness navigation, billing G0023 and G0024 for help “navigating the healthcare system and coordinating care for complex or high-risk conditions”.
While these promising 2024 changes to the Physician Fee Schedule are receiving a lot of attention, neurologists should also look back to the 2015 implementation of the Chronic Care Management (CCM) program. Many specialists assume the program is limited to primary care – but it can also be very helpful for the care of patients who have close relationships with their neurology practices.
Providers can bill for chronic care management (99490, 99439) and complex chronic care management services (99487, 99489) under the CCM program. This program enables neurologists to be fairly compensated for the complex between-visit care they provide their patients with chronic conditions.
Most patients with chronic conditions are in frequent communication with their specialists and have their closest relationships with the specialty practices – potentially talking daily to work through pain management and other symptoms.
Neurology patients expect easy access to information and support from their neurology practices – ideally, two-way texting when they have a question or concern. With demand for neurology services continuing to outpace supply, neurologists can use effective CCM programs to help improve patient access. Many practices are juggling increasingly long average wait times for follow up appointments. Care managers can help by intervening between visits, and by triaging and escalating issues that require urgent attention.
Unfortunately, many neurology practices are unaware that they qualify for a program like CCM or have concerns about overlapping with primary care activities. In fact, specialty practices that implement CCM have enhanced relationships with referring primary care physicians. Those physicians are confident in the care their patients will receive from the specialty practice.
The CCM program is for Traditional Medicare and Medicare Advantage patients. For a typical neurology practice, 1 of 4 of patients may qualify. Patients must be managing two or more chronic conditions that place them at significant risk of death, functional decline, or acute exacerbation or decompensation unless they have a care plan.
Chronic care management programs may be appropriate for patients with:
Many neurology patients have multiple chronic conditions and will have better outcomes under a chronic care management program.
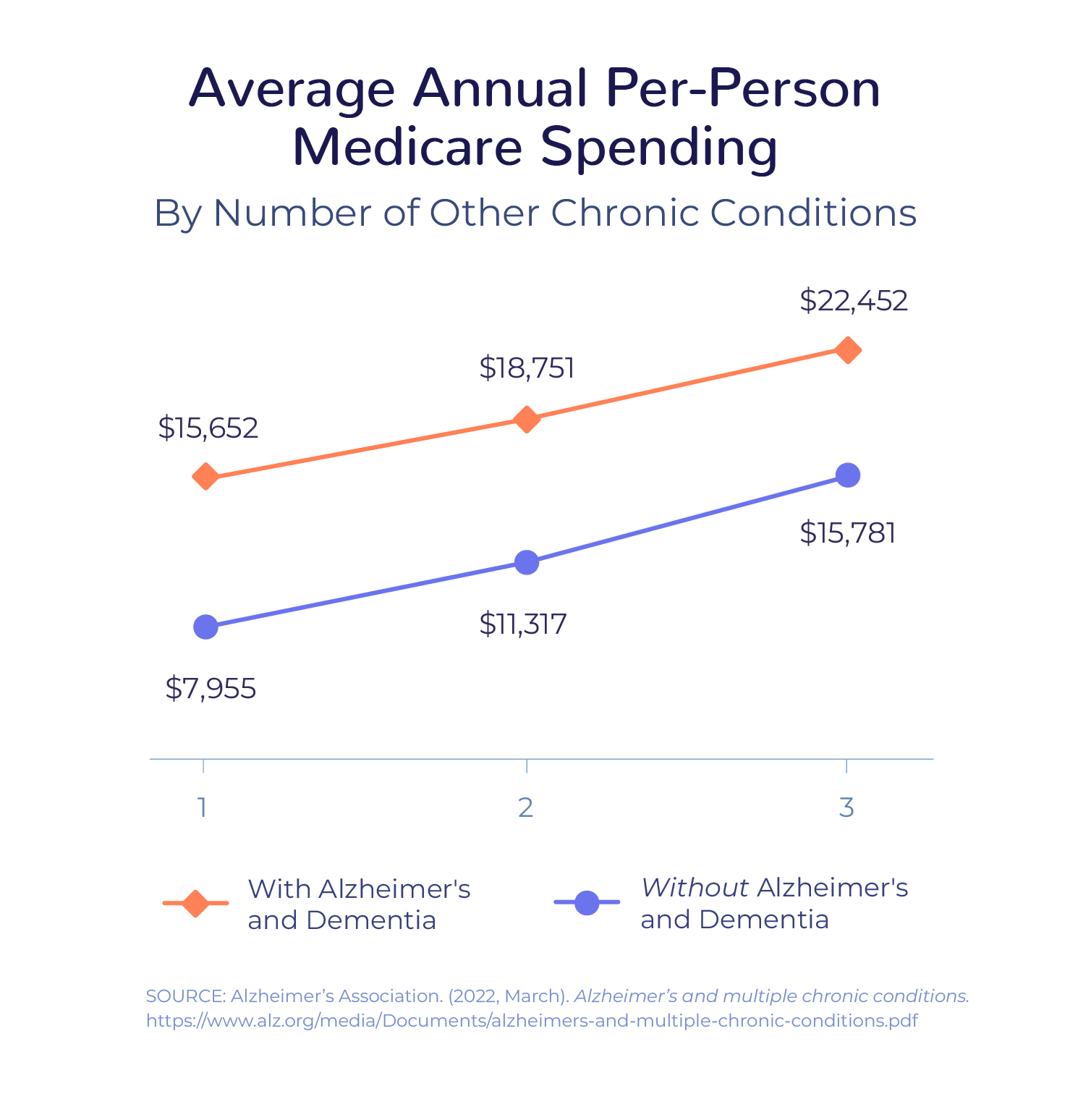
Patients with Alzheimer’s disease and other dementias are much more likely than other patients to have multiple chronic conditions – and those conditions become more difficult to treat as Alzheimer’s disease progresses. More than 95% of these patients have at least one chronic condition, according to the Alzheimer’s Association, and they are 3.8 times more likely to have six or more chronic conditions.
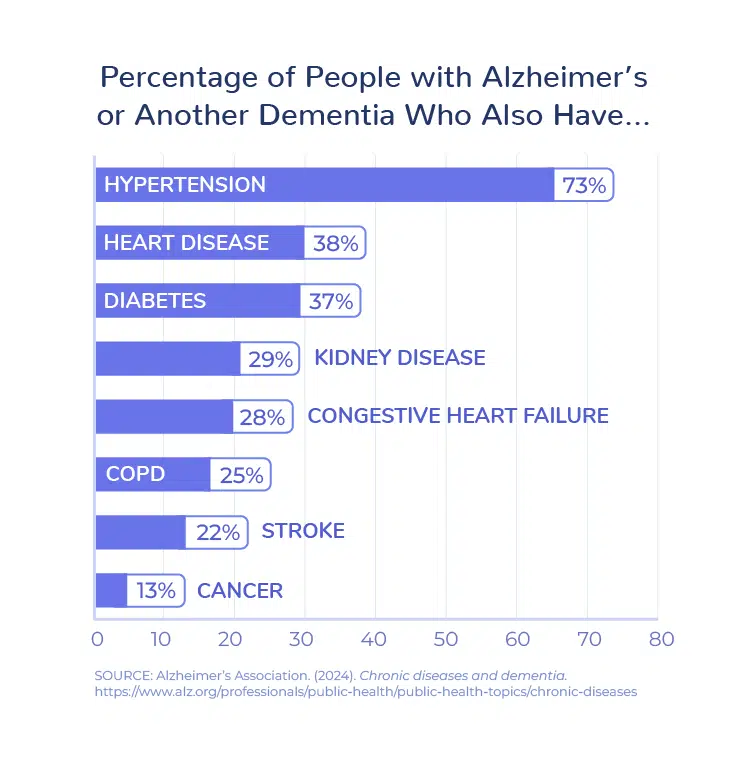
Because Alzheimer’s disease makes it more challenging to manage other conditions, patients are more likely to have preventable hospitalizations. In addition to the strain on patients and their families, preventable hospitalizations and other complications result in significant health care costs – 2.8 times more than for seniors without Alzheimer’s disease and other dementias.
Connecting patients and their families with chronic care management can help neurology practices to identify potential complications and intervene early, avoiding potential hospitalizations and ED visits. Care managers can communicate with caregivers as well as with the patient to ensure the family has all the support they need:
Let’s take a patient who suffered from a stroke and has returned home. The medical team will likely monitor this patient for months and years to help the patient function more effectively, prevent stroke recurrence, and manage complications and other coexisting conditions.
Stroke patients will often have other chronic conditions like hypertension or diabetes. For the patient to have the best quality of life, they will need to stay on medications like antiplatelets or statins, engage in regular exercise, continue physical or occupational therapy, etc. Early detection of cognitive impairment or identification of fall risk factors enables interventions – and regular screenings for depression and anxiety can be particularly important.
When a neurology practice enrolls the patient into a CCM program, the patient gets a care plan and regular engagement with a care manager who can triage and escalate changes in health.
While neurology may not be hit quite as hard as other specialties by the 2024 Medicare fee schedule changes, neurology practices are not immune from rising operating costs, a severe healthcare labor shortage, and the operational challenges associated with the transition to value-based care. The CCM program can be a financial lifeline for neurology practices struggling to manage complex lines of business while delivering substantial between-visit care to patients.
The American Academy of Neurology has an excellent FAQ for practices considering CCM; however, neurologists should also make sure to develop a solid financial and staffing model. (We can help you with this analysis, at no cost or obligation to you.)
A profitable, successful CCM program has the following attributes:
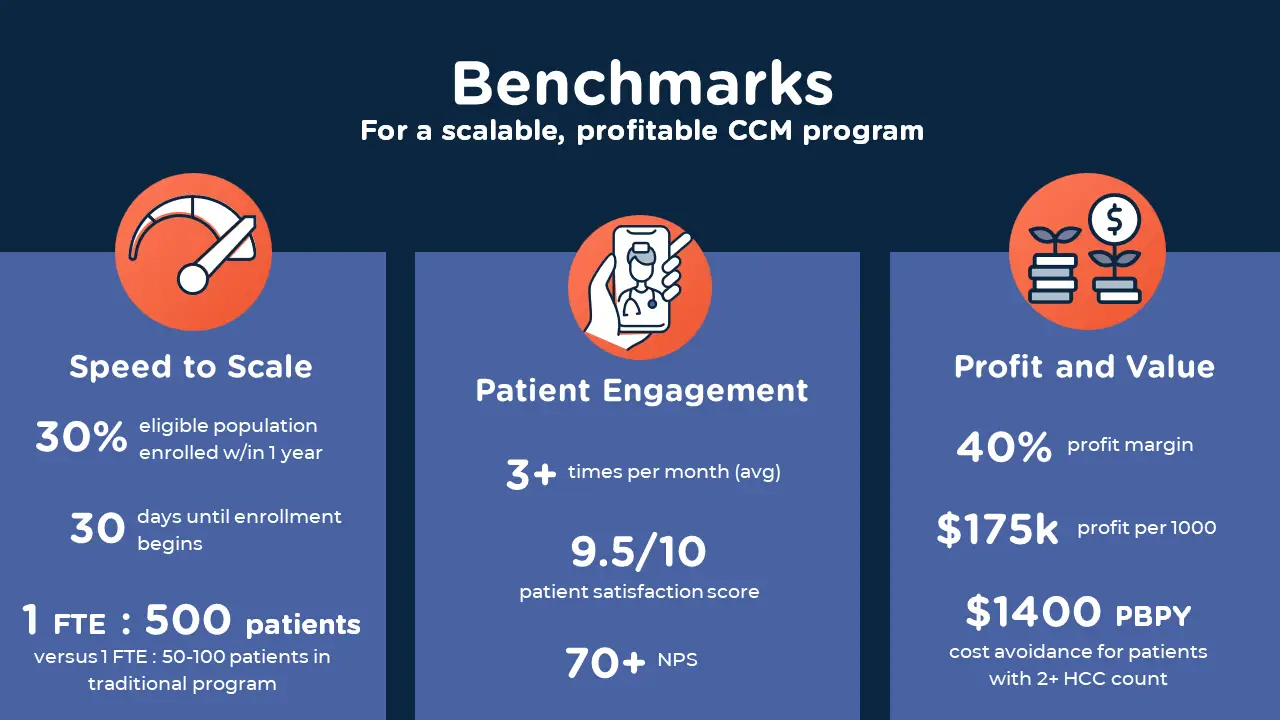
In order to implement a CCM program that achieves these benchmarks, neurology practices need to enable care managers to deliver high-quality care at scale.
Traditional care management programs have a ratio of 1 FTE to 50-100 patients. Given the current labor shortage, implementing a traditional program may severely limit the number of patients who could be enrolled in the CCM program and the impact that program could have.
Neurology practices should explore alternatives to the traditional approach (care managers using an EHR and basic phone system to call patients monthly). Outsourcing is one option, but practices lose direct oversight of care and may jeopardize patient relationships. Keeping the program in-house but supporting the care managers with purpose-built technology can allow for more appropriate clinical oversight, better compliance, and sufficient scale to manage the entire eligible population.