
Last week, I wrote about benchmarking a Chronic Care Management (CCM) program. Because Medicare’s CCM program is severely underpenetrated – only 3% of applicable providers are participating – many medical groups have never had the opportunity to see a scalable, financially sustainable program at work.
Most CCM programs are tiny – an average program size of just 41 patients per provider. This should surprise no one – for decades, care management has been a labor-intensive, expensive service. We treat it like a precious resource to be parceled out to a handful of patients.
Proactive care management is a value-added service for patients, and we would like to provide it to all patients who could benefit. However, care management has historically been a cost center. Today I’d like to address some of the reasons behind that — and challenge whether they are still valid in 2024.
From Meaningful Use to web-based applications to telehealth to AI, technology has transformed healthcare over the past 15 years. Do our assumptions about the scalability of care management still hold water in 2024?
In an on-demand webinar I did recently with the team from Pinnacle Healthcare Consulting, I spoke about some of the challenges with traditional care management. In 2007, the American Association of Managed Care Nurses published guidelines for monthly caseloads based on setting. For disease management, they recommended a caseload of 75-100 patients (acknowledging that geography and patient complexity would also impact caseload size). Other models are consistent with this.
In a traditional model, the care manager has a list of patients to call – and makes three attempts on average before connecting with the patient.
Upon completing the call, the care manager spends typically 20 minutes documenting the call in the EHR. These tedious administrative tasks can lead to burnout and staff turnover.
Healthcare finance expert Lucas Hutchison, MHA tells us that labor costs are 84.8% of total expenses – up from 82.4% in 2021. Medical groups are struggling to retain staff amidst a widespread labor shortage.
Meanwhile, physicians are squeezed by margin compression. Between 2001-2020, Hutchison tells us that costs increased 38% while reimbursement increased only 8%. Physicians and advanced practice providers are working harder – seeing more patients – to stabilize their practice financially.
In this economic climate, it can be untenable for medical groups to invest in proactive chronic care management. When a care manager’s panel is 50-100 patients, the cost is simply too high.
The inefficiency of the traditional model means that many patients receive a check-in call once per month.
These limited interactions are often rote or scripted – or too infrequent for the patient to build a trusted relationship with the practice. This reduces the amount care managers learn about the patient’s needs – especially when sensitive social determinants of health (SDoH) factors are interfering with the patient’s ability to achieve health outcomes.
And when the frequency of interaction is so low, the chance of doing early detection and early intervention is also very low. Let’s say a care manager checks in with a patient on February 19th, and then again on March 19th. In the intervening 30 day period, the patient may experience worsening symptoms. You cannot rely on the patient to reach out to you unless the patient has an easy, frictionless way to reach out to your practice.
As an industry, we talk about the importance of proactive care – but is that actually what we get with the traditional model of care management? Many patients could benefit, but few are actually enrolled.
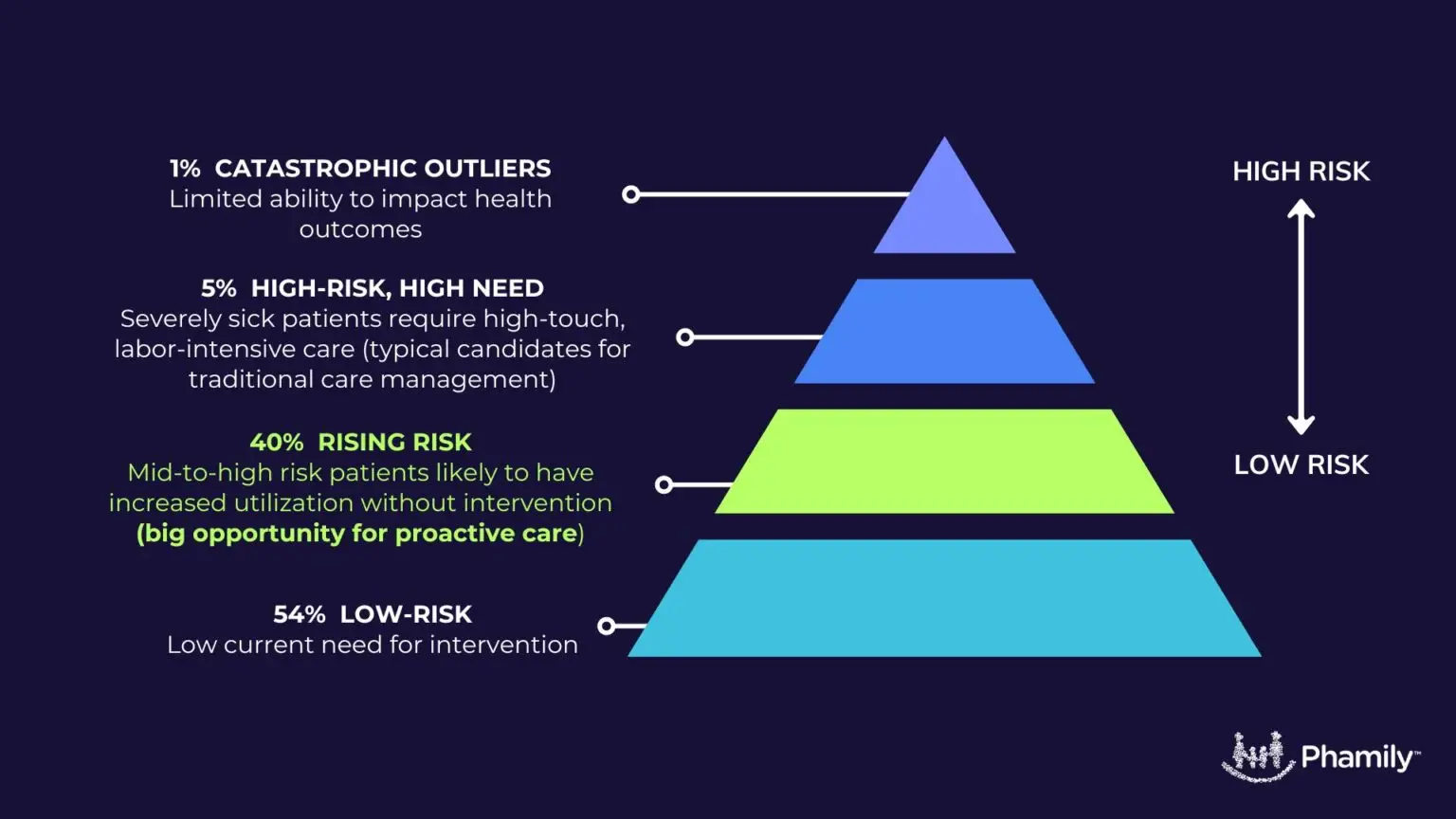
When we assume care management is a costly resource, we spend substantial effort identifying the limited cohort of patients to enroll. Typically, these patients are high risk and have had triggering events that flag them for care management. We are reactive instead of proactive – i.e. we are reacting to a patient’s heart attack with a care plan instead of working with the patient to prevent the heart attack in the first place.
If we discard the assumption that we can only support a limited number of patients with a care management program, we can expand care management services to patients with rising risk who have not yet had critical events.
In order to expand the patients who can benefit from proactive care management, we need to make care management economically feasible for medical groups. How can existing staff increase panel size to the point where the economics work – without burning out?
The answer is the careful application of technology – something for which we are uniquely positioned in 2024.
When we deploy technology intelligently, we can make care managers 10x more efficient. This means that a small practice with two care managers can provide proactive care to 1000 patients instead of 100 patients – and be profitably reimbursed for those activities.
So how do we do this? In my next article, I’ll explain how care management can scale up while becoming financially sustainable for medical groups. But for now, let me ask you:

Darshan has 15+ years experience co-founding and building high growth healthcare technology businesses committed to improving access to care and quality of care. More about Darshan…