
Medicare will begin reimbursing providers for Advanced Primary Care Management (APCM) in 2025, and many providers are trying to decide whether to take advantage of this program. Will you be able to operate cost-effectively? What does it mean to provide “24 x 7 access”?
But as you work through these details, don’t forget why Medicare launched the program. Care management that actually engages and activates patients is key to better health outcomes and is the core of APCM.
Success under APCM means creating value for all stakeholders: your practice, Medicare (and taxpayers), and your patients.
If you are going to do this right, there are no hacks, and no gimmicks. You cannot take a “check the box” approach. You need to deliver great care management at scale.
With APCM, Medicare wants you to assume holistic responsibility over your patient’s primary care. By definition, that means it is insufficient to only take care of the patient during the 4 days of the year they visit your office.
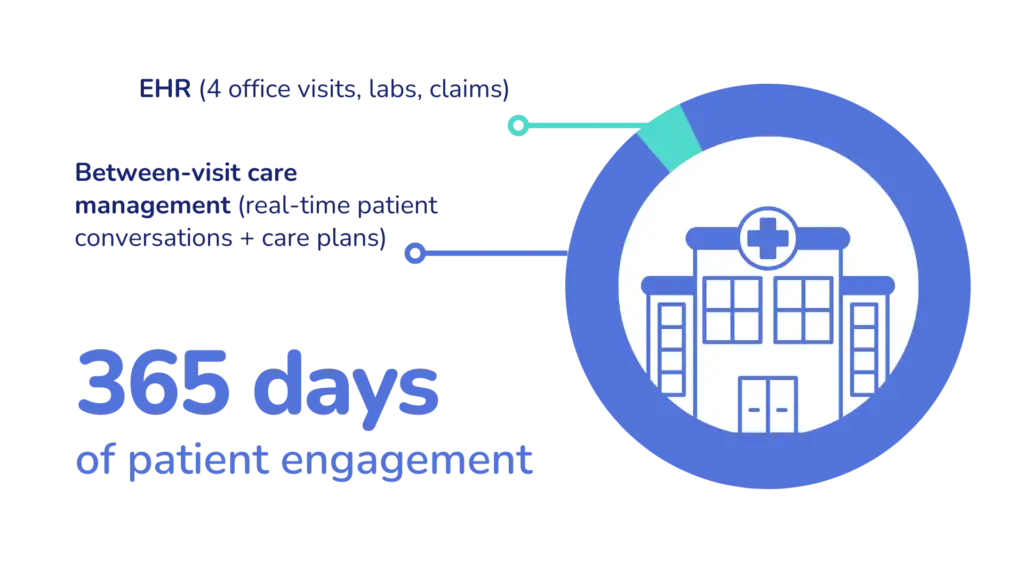
You must engage your patients the other 361 days of the year. You cannot wait for them to reach out to you. Rather, you need to take a proactive stance with consistent and frequent patient engagement.
The cornerstone of APCM is consistent, proactive care delivered at scale (to thousands or tens of thousands of Medicare patients) in a way that actually adds value to your patients, to your payors, and to your organization.
Technically, you could bill APCM for every patient every month. But you have to ask yourself: Is that a smart strategy? Will it create value for all stakeholders? Will it be sustainable?
Remember that many patients will have a cost sharing responsibility. It’s essential that you are not just “checking the box” but that you actually deliver high quality care management. And moreover, you need to ensure your patients understand the value of that care.
With over a decade of experience building large-scale Chronic Care Management (CCM) programs, we know that there is a virtuous cycle that drives CCM program success. That same cycle will drive APCM program growth.
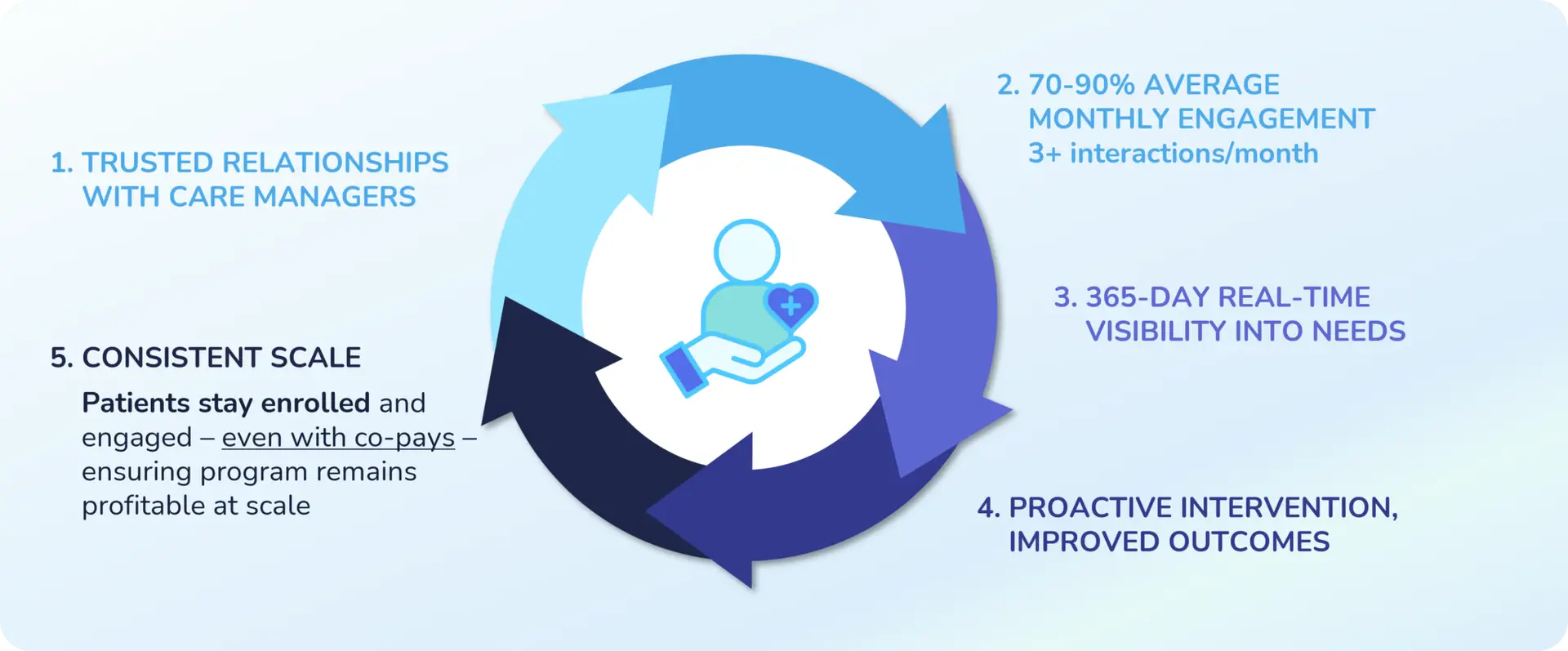
Every month, a successful proactive care program – either CCM or APCM:
Over time, this virtuous cycle has enabled hundreds of healthcare organizations to scale their proactive care capabilities using CCM reimbursement – and the model will support APCM as well.
Let’s talk more about how you can actually deliver high-quality care at scale.
Care management programs often fail because they are not staffed with dedicated resources. When care managers are also supporting front office operations or providing in-office patient care, the care management program suffers.
Make sure that your care management team is fully dedicated to care management, so that they are able to develop trusted relationships with their patient panels.
Consistent, proactive outreaches from care managers will enable you to get in front of patient needs and deliver proactive interventions. This will ultimately lead to better health outcomes and reduced hospital visits.
In order to do this at scale, your care managers will need the right tools. Especially important are simple, guided workflows that help them take the next best action hour-by-hour, day-by-day.
CCM requires 20+ minutes of care to be delivered in a given month in order to submit a claim for reimbursement. But with APCM, there are no time tracking requirements.
This opens up an opportunity to leverage automation and AI to achieve extraordinary operational efficiency. You can arm your care managers with “superpowers” and enable them to handle larger case loads without sacrificing care quality. AI can help care managers increase consistency and adherence to best practices.
This is how you can achieve caseloads of 1:1000 or 1:2500 while delivering consistent value to patients (keeping them in the program), ensure a profitable program, and ultimately improve health and cost outcomes.
If you’d like more information about APCM versus CCM, I encourage you to register below for our webinar. We’ll talk with Tracie Jefferson, PA-C, the Quality Director at Sound Family Medicine, about why her practice has decided to move from CCM to APCM.
WEBINAR
With the Centers for Medicare & Medicaid Services’ recent introduction of reimbursement for Advanced Primary Care Management (APCM), administrators and physician leaders face important decisions: Should you leverage CCM or explore APCM for your practice?
Join us for an insightful webinar designed for managing partners, practice administrators at physician groups and physician leaders and administrators at health systems.
We’ll unpack the differences between CCM and APCM, discuss their implications, and help you start thinking about the right fit for your organization.

Darshan has 15+ years experience co-founding and building high growth healthcare technology businesses committed to improving access to care and quality of care. More about Darshan…